Living Well with Cancer

Report Summary
In 2024 Healthwatch Shropshire engaged with 390 people about living with and beyond cancer, including :
- 40 people who completed our online survey
- 226 people who we spoke to face-to-face at cancer support groups and Cancer Champion meetings across Shropshire
- 115 people who we spoke to at local Cancer events
- Nine professionals working directly with people with lived experience of cancer or responsible for implementing the NHS Shropshire Telford and Wrekin Integrated Cancer Strategy 2022-27 to ensure the views of the people we heard from would be taken into account.
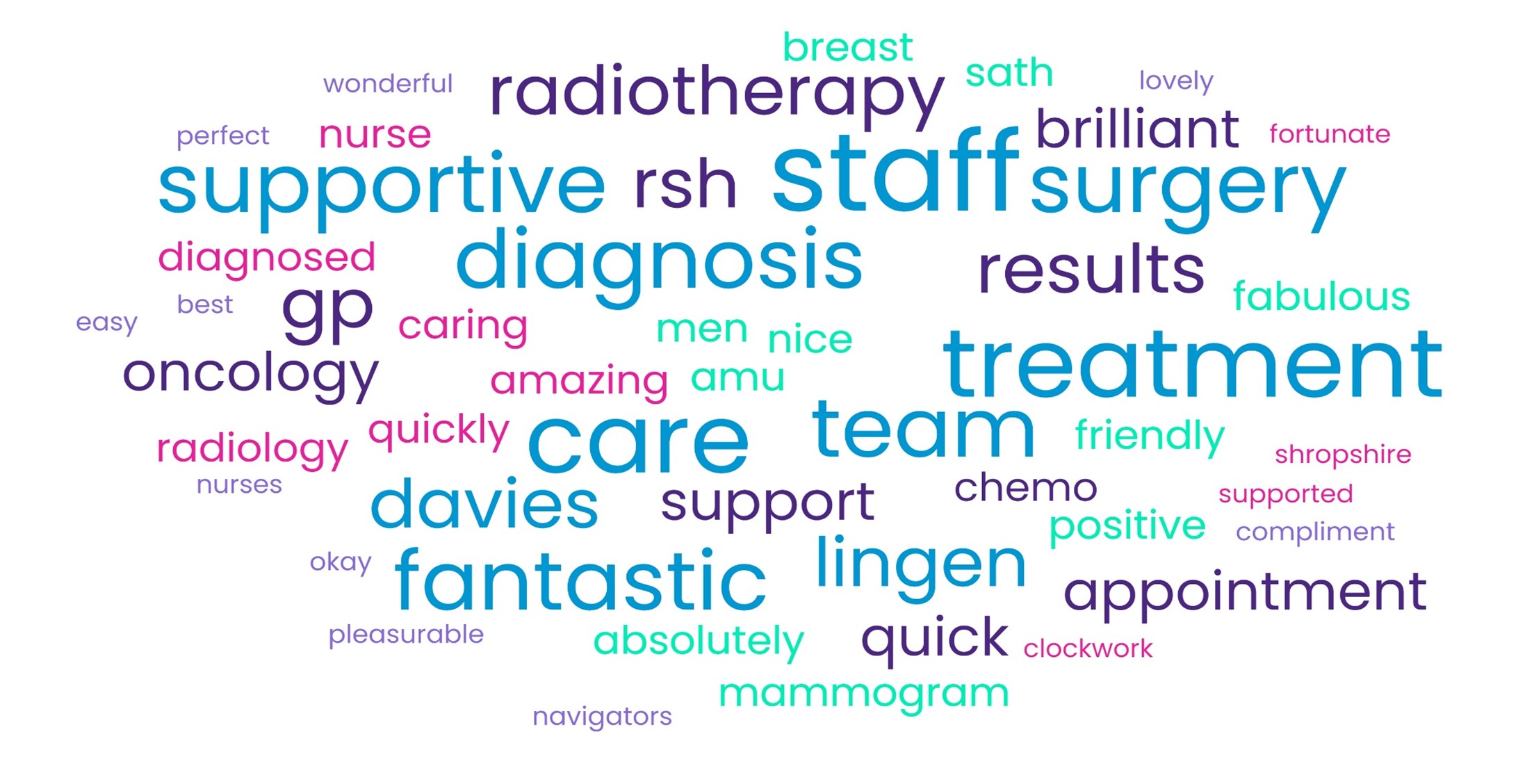
What’s working well
Many people shared their positive experiences of cancer services and the non-NHS support available from local and national organisations and community cancer support groups.
"There are pockets of excellence in the system but there are also gaps in care that could be improved." (Survey respondent)
What would support people to live with and beyond cancer? – Key messages
We also asked people to share with us when things had not gone so well or not gone as they had hoped/expected and their suggestions for improvement.
These can be grouped under the following 10 key points, supported by sample quotes:
1. More personalised support from medical professionals to help patients access information about their condition, treatment and support available (including signposting)
‘Listen to individual circumstances.’
‘Read notes and have some kind of understanding before the appointment. She [carried on] without knowing anything of me as an individual.’
‘It would be nice to be able to access blood test results remotely via a website or app so I am able to see them on a monthly basis.’
2. Need for improved communication with patients (including understanding and empathy)
‘Talk to the patient, don’t assume they won’t understand and give them a chance to have someone with them.’
‘It would be great if you could be contacted as soon as your results come in – I for one would be happy with a phone call whatever the results. Ask us.’
‘Remind staff that the people they are seeing are human beings and being told you have cancer is devastating.’
3. Consider the amount, quality and timing of information given to patients after diagnosis
‘I would have appreciated being given time for information to sink in then a special session for me to ask questions in regard to my specific condition and the future.’
‘Lots of leaflets given to read on first appointment. This was overwhelming. So much so that I couldn’t read it all until recently. Would have been better with targeted information face-to-face on simple things, e.g. things I needed post-surgery and possible problems after surgery.’
4. Improved clinical support for patients after diagnosis, treatment / discharge (including increased staffing)
‘Seeing a doctor more often. Having more physical examinations to reassure you that everything is OK.’
‘Reinstate funding for the post.’
‘More support for young women enduring hormonal treatment.’
5. Improved access to additional emotional/wellbeing support and other therapies, including groups/workshops that promote exercise and wellbeing for people living with and beyond cancer (consider terminology, e.g. ‘counselling’)
‘It's a very difficult process and such a big psychological change I think they need to intervene earlier with alternatives to medical treatment.’
‘I really enjoyed the make-up session, you felt so good, we wanted to go out afterwards.’
6. Personalised support and information for families and carers (including at end of life)
‘Remember the partners are the patients support network.’
‘Having a link and communicating to immediate family whilst in hospital would be advantageous.’
7. Need for improved communication and joint working between professionals to make sure people are diagnosed early and have access to the right treatment at the right time, and things go smoothly (including improved waiting times and access to parking permits at the hospital)
‘Chemo should have started sooner and GP should have acted more quickly on health struggles I was having.’
‘Just do your job in a timely manner… that’s all I ask.’
‘Improve waiting times for GPs to answer calls.’
8. Need for a Shropshire Cancer Network, recognising the importance of community groups and their funding challenges - supported by accurate information and directories for the public and professionals so everyone knows the support is available and how to access it.
‘If one type of cancer patients needs post-surgery support, then why not everyone?’
‘Everyone is so focused on what they are doing, there isn’t anyone bringing us all together, we don’t know what else is out there’.
Support groups
As we met groups from across Shropshire we heard a huge amount of positive feedback about people running community-led support group, their determination and passion about what they do, for example:
“There is one person to thank for all of this and that is [], she is a force to be reckoned with but for all the right reasons. We have a lot to thank [her] for. The group is independent of any national charity yet manages to raise thousands of pounds a year for other cancer charities. I’m so proud of the group. Many hours of work by [] and the committee. They were encouraged by our local councillor [] It was her idea to apply. The work continues and the support for people and families who are affected by cancer is now forming a strong network in the South Shropshire area.”
Downloads
If you would like this report in an alternative format or if you have any questions regarding it please Contact Us
